
Photo: Lagan Valley Freestanding Maternity Unit
Midwifery Units in Northern Ireland
By Seána Talbot
There were 24,394 live births in NI during 2014 (NISRA, 2015) with the total number of MLU births being 2,960 – equating to 12% of births. The home birth rate is stubbornly bottoming along at less than 1% (n=67).
NICE guidelines advise health care professionals working with low-risk women to:
- Explain to both multiparous and nulliparous women that they may choose any birth setting (home, freestanding midwifery unit, alongside midwifery unit or obstetric unit), and support them in their choice of setting wherever they choose to give birth:
- Advise low-risk multiparous women that planning to give birth at home or in a midwifery-led unit (freestanding or alongside) is particularly suitable for them because the rate of interventions is lower and the outcome for the baby is no different compared with an obstetric unit.
- Advise low-risk nulliparous women that planning to give birth in a midwifery-led unit (freestanding or alongside) is particularly suitable for them because the rate of interventions is lower and the outcome for the baby is no different compared with an obstetric unit.
NICE Guideline CG190, Intrapartum Care for Healthy Women and Babies, December 2014
Despite this, a quick glance at the NI Midwifery Unit map shows that, unless a woman lives in greater Belfast, her choices are currently limited.
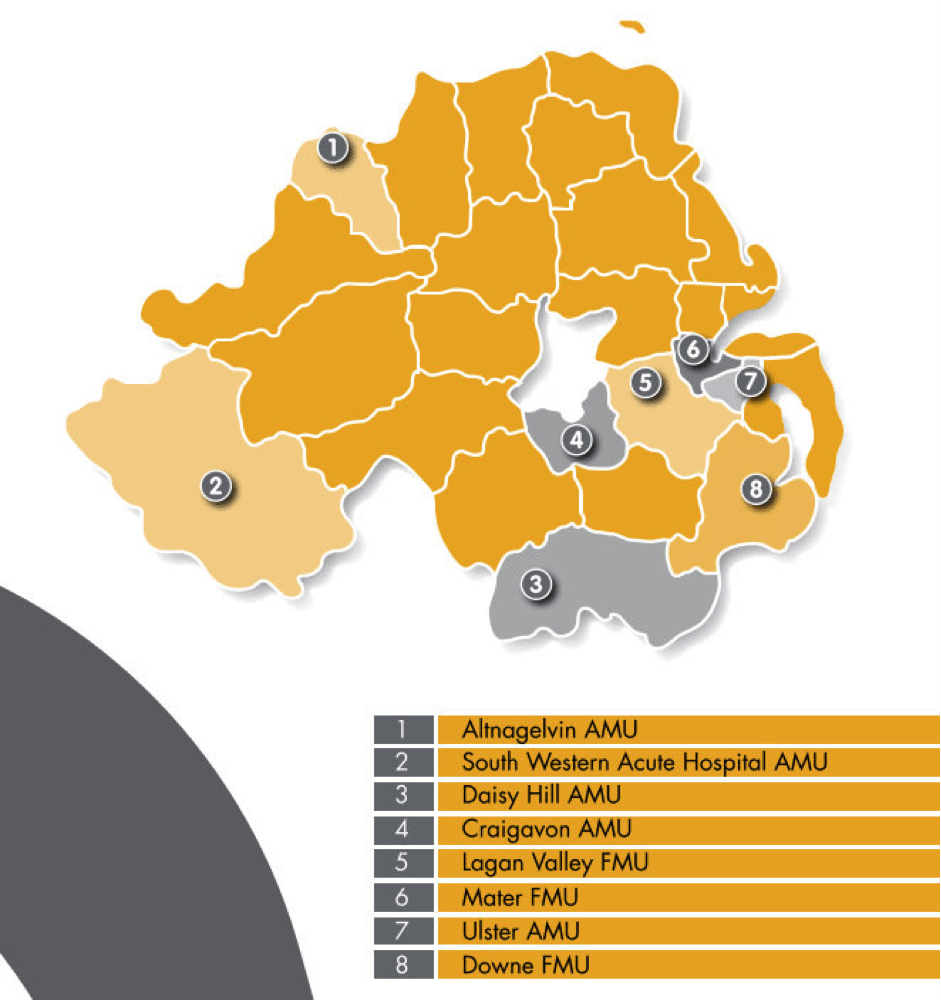
Currently, there are three freestanding and five alongside units, with a further alongside unit in development in Belfast. The units are geographically clustered in the east, and (apart from the Downe and the South Western units) in areas of higher population density, so women living on the north coast, west of Lough Neagh, or in rural areas have limited options.
Our maternity strategy commits the Health & Social Care system in N Ireland to ensuring that women have access to midwifery-led options as part of a wider culture change. Units are also known as MLUs (midwifery led units) in Northern Ireland.
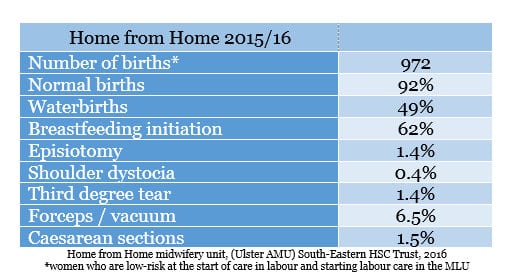
Our midwifery units are highly valued by the women who use them. A quick look at some of the outcomes from one of the units indicates some of the reasons why:
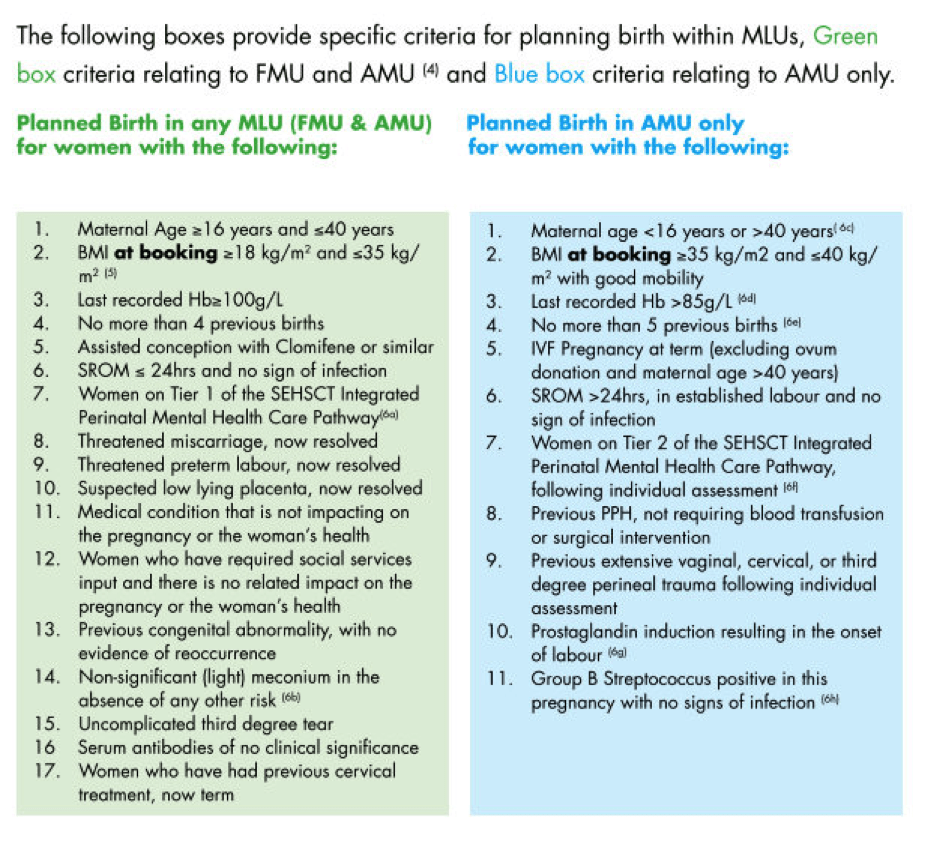
In NI, eligibility criteria are used as a screening tool for admission in line with accepted practice elsewhere. Each MLU in NI had developed their own admission criteria to guide both maternity care professionals and women. In practice, this meant that there was a lack of consistency across NI, as the differences in the criteria and their application impacted on women’s planned place of birth. This led to some women being either inappropriately refused admission to the MLU, incorrectly admitted to a MLU, or transferred unnecessarily to an obstetric unit.
It was also recognised that the admission criteria varied from one MLU to another, were often not clearly defined, and that midwives in NI had expressed the need for clear evidenced-based guidelines (Healy, 2013).
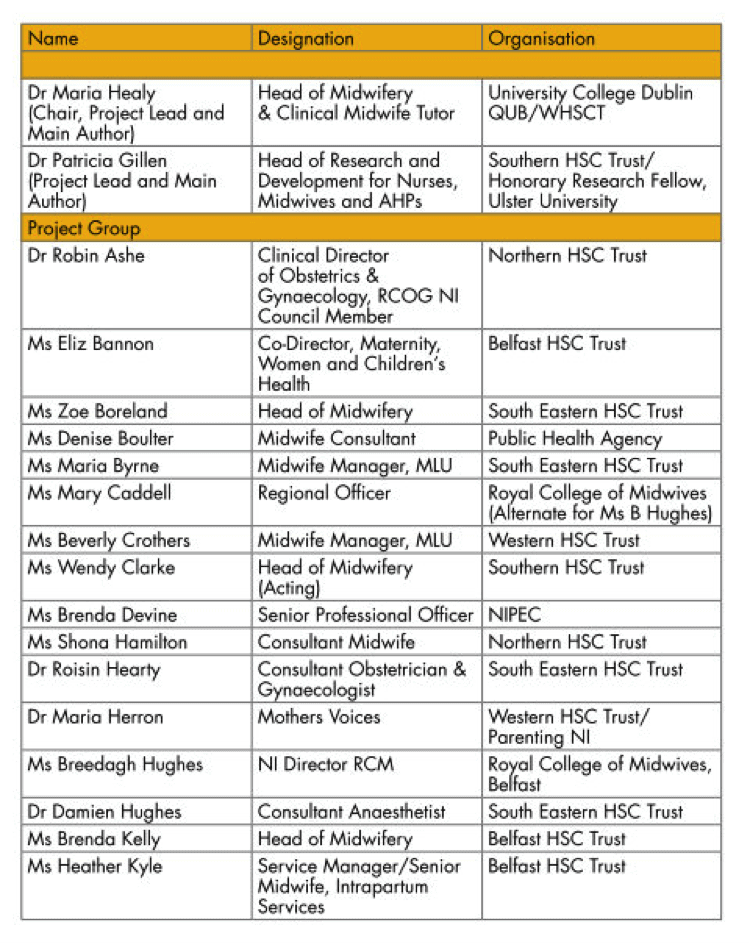
The Guidelines and Audit Implementation Network (GAIN) is the body which produces official clinical guidelines for use in Northern Ireland. In 2015, the network completed a detailed guideline document for midwife led units. The process was thorough and at times challenging, and involved multidisciplinary and service user guideline development group members reviewing the available evidence and building a consensus about which women should be encouraged to choose midwifery units for their birth. The group included practising midwives, lecturers and researchers as well as obstetricians, GPs, anaesthetists and, importantly, women and women’s advocates. The results of the Ten Thousand Voices listening project, which included maternity care, was also influential in shaping the work.
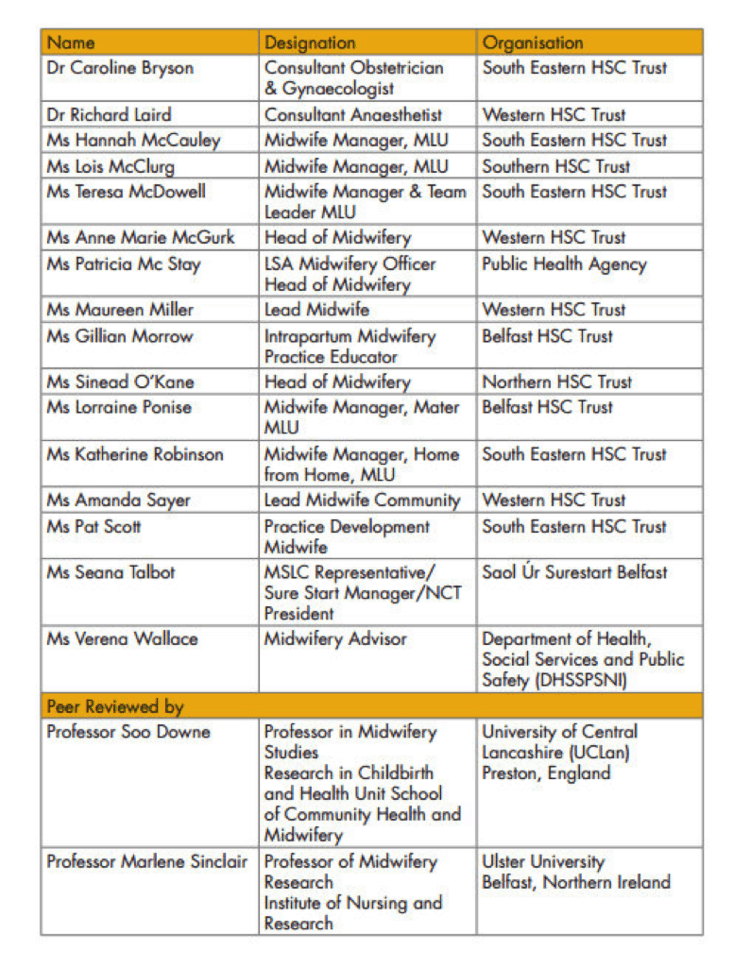
Initially, the plan was to produce a single list of criteria to guide women and health care professionals. However, as well as agreeing a core list, applicable to both alongside (AMU) and freestanding midwife led units (FMU), the group identified another group of women, with a slightly higher risk profile, who should be encouraged to attend alongside midwifery units only.
In addition, the group identified that more women than expected were transferring out of midwifery units to consultant units while in labour. In order to reduce the numbers of unnecessary transfers out, the group developed a Normal Birth Care Pathway. The pathway focused on confirming that women are in established labour before admission to the unit in labour, as well as identifying best practice in terms of supporting women experiencing straightforward labour.
The guidelines and pathway are available online HERE
In order to encourage implementation of the guidelines, the Chief Nursing Officer has supported the roll-out of awareness sessions for midwives in all Trusts in NI. A detailed evaluation is planned for 2018.
Details of the individual units can be found on the various Trust websites
1. Altnagelvin AMU Check out video which covers obstetric as well as midwifery led options
2. South Western Acute Hospital Check out video which covers obstetric as well as midwifery led options
3. Daisy Hill Hospital AMU Check out video
4. Craigavon Area Hospital AMU Check out video
7. Ulster Hospital Home from Home AMU Check out video
8. Downe FMU

Photo: Lagan Valley Freestanding Maternity Unit


I was low risk at first birth but wanted consultant led care. The only option available to me on the NHS was community midwife antenatal. I had to pay for the treatment I wanted and certainly did not feel like I was either being offered or had a choice outside of paying privately. Consultant led care is a valid choice for some women and I often felt choice was only available to those who were interested in going down the currently popular route towards non medicalised birth.
Thanks for your comment Jayne – our aspiration is for all healthy women who aren’t expecting complications to be offered the choice of an MLU, regardless of their postcode.